Endometriosis: It's Not Just Painful Periods
Many women think that period pain is normal but if the pain is so bad that it keeps someone from going to work, school, having relationships, or living their daily life, there may be something else going on. Endometriosis is a long-term inflammatory disease that affects about one in ten women of childbearing age.
Endometriosis is a lot more than just "bad cramps." It is a complicated medical condition that can affect your physical health, emotional health, ability to have children, and quality of life in general. Having chronic pain and trouble getting pregnant can be hard on your mental health. A lot of women have anxiety, depression, or feel alone. Support is very important for healing, whether it comes from counseling, community groups, or loved ones.
It is a real medical problem that needs to be looked at, understood, and treated right away. Women who report intense menstrual pain or ongoing pelvic symptoms must not be disregarded. Recognizing and managing the problem early on can greatly improve quality of life and fertility outcomes.
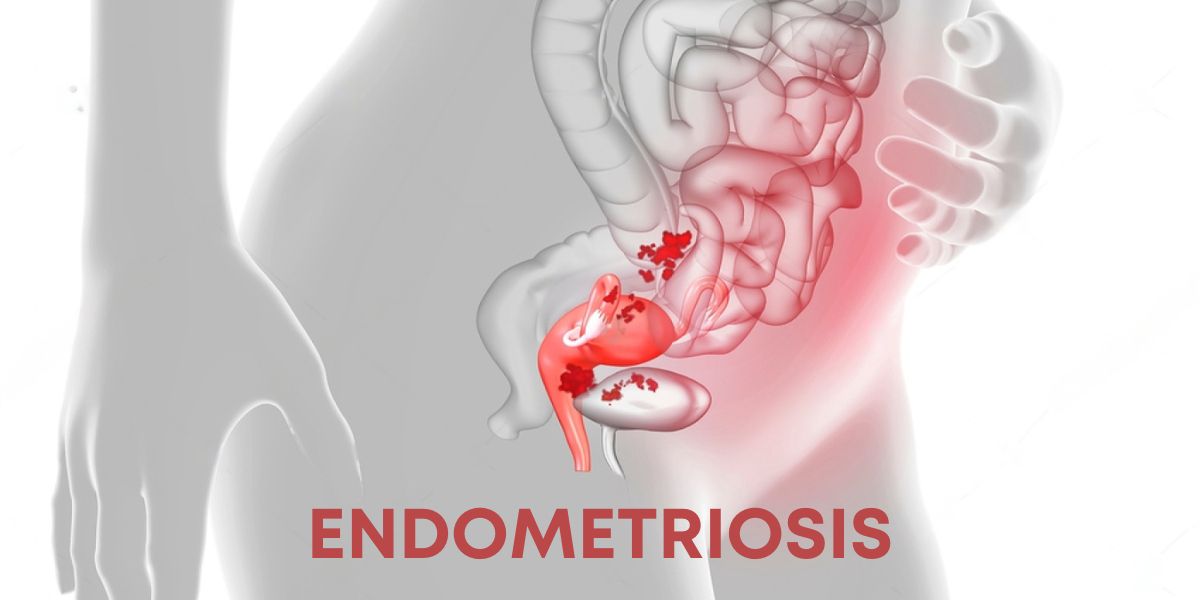
What is endometriosis?
Endometriosis happens when tissue that is like the lining of the uterus, called the endometrium, starts to grow outside of the uterus. These tissue implants can show up in the ovaries, fallopian tubes, pelvic wall, bladder, bowel, or, in rare cases, outside the pelvic area.
These implants react to hormonal changes that happen every month, just like normal uterine tissue. They get bigger, fall apart, and bleed. But this trapped blood doesn't have anywhere to go, which causes:
• Inflammation
• Making scar tissue
• Adhesions (when organs stick together)
• Pain that is severe and long-lasting
The progression differs significantly. Some women have a lot of disease but not much pain, while others have very bad symptoms even with very few lesions.
Signs: It's Not Only About the Time
Pain during your period is a common sign of endometriosis, but the pain is different. It can start before your period, last through it, and go on for a long time after it ends.
Some common signs are:
1. Pain in the pelvis
Persistent, throbbing, or sharp pelvic pain that may get worse during your period.
2. Painful sex
Many people don't realize that deep pain during or after sex is a common sign of endometriosis.
3. Painful bowel movements or urination
Especially when you have your period, because of implants in the bladder or bowel.
4. Periods that are heavy or not regular
Bleeding that makes it hard to do everyday things.
5. Infertility: Endometriosis is one of the main reasons why women have trouble getting pregnant. It affects about 30–40% of women who are trying to get pregnant.
6. Tiredness, bloating, and nausea
Many women talk about endo-belly, which is painful bloating that can happen all of a sudden.
Because these symptoms are similar to those of PCOS, IBS, pelvic infections, or hormonal imbalance, it's easy to get the wrong diagnosis. Women usually have to wait 7 to 10 years before they get the right diagnosis.
Why people often get endometriosis wrong?
People and the healthcare system often downplay endometriosis because:
• They think period pain is normal
• Patients and sometimes even providers don't know much about it
• Symptoms can be very different from person to person
• Signs can be similar to those of other disorders
This makes a lot of women feel like they aren't being heard or taken seriously, which can delay getting the right care.
How do doctors find out if someone has endometriosis?
A combination of clinical evaluation, symptom assessment, and imaging tests is used to make a diagnosis. Laparoscopy is still the best way to find ovarian cysts called endometriomas, even though ultrasound can do it. This minimally invasive surgery lets you see and remove endometriosis lesions to confirm the diagnosis.
It is important to find out about the condition early because it can get worse over time and affect fertility.
Choices for Treatment
There is no one treatment that works for everyone with endometriosis, but there are many that can help with symptoms, stop the disease from getting worse, and help with fertility.
1. Managing Pain
Pain-relieving drugs and NSAIDs can help with inflammation and pain.
2. Hormonal Therapy
• Birth control pills
• Progesterone
• Hormonal IUD
• GnRH agonists
These work by controlling the hormonal cycle and slowing down the growth of the implant.
3. Surgery with a laparoscope
Removing lesions, cysts, or adhesions through surgery can greatly reduce pain and increase fertility.
4. Lifestyle and Supportive Approaches
• Diet that fights inflammation
• Physiotherapy for pelvic floor dysfunction
• Yoga and light exercise
• Managing stress and sleep
The best results usually come from a mix of medical and holistic care.
If you or someone you know has symptoms that make it hard to go about your daily life, see a gynecologist and get a proper evaluation. The best way to get an early diagnosis and better treatment is to talk about your menstrual health.